ọdịnaya
Many patients, sometimes even after undergoing the mild form of COVID-19, have long-term problems with concentration disorders, pain in the chest, muscles, joints, breathing problems, fatigue and other symptoms. This is called long COVID, which fortunately is getting better and better understood.
- Scientists from the University of the West of Scotland have counted as many as 100 possible symptoms of long COVID!
- The symptoms of long COVID include: trouble thinking (brain fog), pain in the chest, abdomen, headache, joint pain, tingling, sleep disturbances, diarrhea
- Scientists alert that the long-term effects of the COVID-19 transition are emerging on such a scale that they may exceed the capacity of healthcare systems
- Scientists are beginning to recognize risk factors for long COVID. What is already known who is most at risk?
- Enwere ike ịchọta ozi ndị ọzọ na ibe mbụ Onet
John is a middle-aged man who was healthy and in full strength two years ago. Now even gentle, sports games with children must be carefully planned in order to have a lot of time to recover later. A year ago, he even had a hard time reading fairy tales to children before bedtime. This is how he recently described his story for the BBC. Why has his health deteriorated so much? The cause was SARS-CoV-2 infection. Even though it was gentle, John now suffers from so-called long COVID. There are many more people like that.
What are the symptoms of Long COVID?
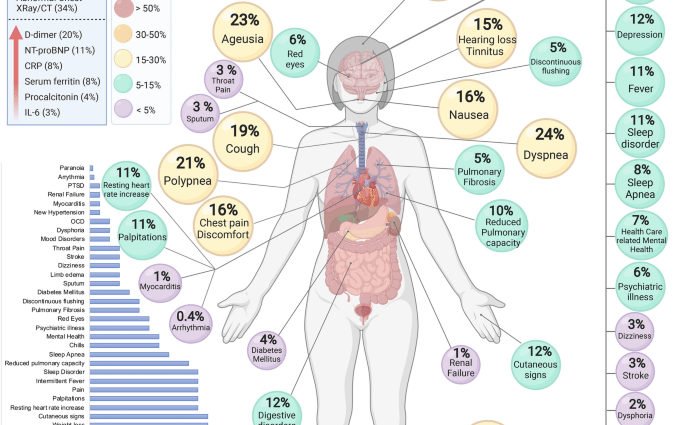
The American agency Centers for Disease Control and Prevention provides a long list of the most common complications that can occur in such people, often several of them at the same time. It includes:
nsogbu iku ume
ụkwara
ike ọgwụgwụ
deterioration after physical or mental exertion
trouble thinking (brain fog)
pains in the chest, abdomen, headaches, joint pains
tingling
osooso onu ogugu obi
afọ ọsịsa
nsogbu ụra
ọkụ
dizziness
rashes
ngbanwe ọnọdụ
nsogbu na isi ma ọ bụ uto
menstrual disorders in women
Researchers from the University of the West of Scotland, in an analysis of available studies, presented in the last fall of last year in the journal “Frontiers in medicine”, counted as many as 100 possible symptoms of long COVID!
Ihe odide ndị ọzọ dị n'okpuru vidiyo.
SARS-CoV2 – raid on the body
Maybe this shouldn’t come as a surprise given that COVID-19 affects many organs, including the heart, lungs, kidneys, skin, and the brain. And it works in different ways. In addition to the damage caused by the virus itself, dangerous inflammation occurs. Clots may also appear, not only the very dangerous ones, e.g. related to a stroke or heart attack, but also smaller ones that block small vessels and damage the heart, lungs, liver and kidneys.
Vascular tightness and the blood-brain barrier may also suffer. The infection can also provoke tissue damaging autoimmune reactions. All this is combined with the effects of sometimes extremely high stress associated with hospitalization, burdening treatment, and in some cases even life-threatening. Some people may even develop post-traumatic stress disorder. These problems make diagnosis and treatment more difficult.
Long COVID: Prevalence
Many are sick. According to data published in March by the British Office for National Statistics, 1,5 million people in Great Britain, while already living in their own homes, experienced long COVID, that’s 2,4 percent. population.
Researchers at Penn State College of Medicine, after analyzing 57 studies related to long COVID, involving 250. survivors, noticed that at least one symptom of this syndrome, even six months after infection, affects 54 percent. such people. The most common are movement disorders, lung function disorders and mental problems. It should be noted, however, that almost 80 percent. participants of these studies were seriously ill and hospitalized.
Scientists warn: “The long-term effects of the COVID-19 transition are emerging on such a scale that they may exceed the capabilities of health systems, especially in low- and middle-income countries.”
Who is most at risk of long COVID?
While it often seems that health and illness are a lottery, problems usually have specific causes. Scientists are also starting to recognize risk factors for long COVID. The authors of a study published recently in the journal Cell, after observing several hundred sick and several hundred healthy people, discovered several parameters that increase the risk.
They were most raised by the presence of some autoantibodies, e.g. related to rheumatoid arthritis. The amount of viral RNA at the time of infection also mattered – the more viruses in the body, the greater the risk of complications. It also increased if the Epstein-Barr virus, which infects most of the human population over the course of its life, reactivated (but most often remains hidden in the body unless it becomes seriously ill).
Diabetes is another important risk factor. In addition, women with chronic obstructive pulmonary disease were more likely to suffer from long COVID.
It should also be noted that in this study the majority (70%) of the population included in the study was hospitalized due to COVID-19, which indicates that the researchers analyzed the group with a clear predominance of patients with severe disease. However, researchers noted that similar trends apply to people who have had the disease more mildly.
Ọ bụrụ na ị nwere COVID-19, jide n'aka na ị ga-anwale. Ngwungwu ule ọbara maka convalescents dị Ebe a
The latest data also indicate the possible importance of the virus variant as a risk factor for long COVID. This was recently reported by a team from the University of Florence during the European Congress of Clinical Microbiology & Infectious Diseases. Researchers compared the symptoms present in people suffering from COVID-19 when the primary variant of the virus was dominant with complications in those affected by the action of mainly the alpha variant. In the latter case, muscle aches, insomnia, anxiety and depression were less frequent. However, there were more frequent changes in the sense of smell, difficulty swallowing, and decreased hearing.
‘Many of the symptoms noted in this study have been seen before, but this is the first time they have been associated with variants of the virus that causes COVID-19,’ said author of the finding, Dr Michele Spinicci.
At the same time, this study found that people with type 2 diabetes had a lower risk of developing complications.
– The long duration and wide range of symptoms show that the problem will not go away easily and more action is needed to help patients in the long term. Future research should focus on the potential impact of different variants on the condition of patients and check the effects of vaccinations, adds the specialist.
Vaccinations protect against long COVID
The importance of vaccination in relation to long-term COVID has been explored by the authors of a study recently published by the UK Health Security Agency. They analyzed the results of 15 studies in this area.
“Evidence shows that vaccinated people who later become infected with SARS-CoV-2 are less likely to report symptoms of long-term COVID than unvaccinated people. This applies to both the short time scales (four weeks after infection), the medium (12-20 weeks) and the long (six months), the researchers write.
Fully vaccinated survivors were approximately half as likely to be affected by long-term COVID as unvaccinated survivors. Experts point out that in addition to these benefits are vaccine-induced protection against the infection itself. Some studies also show that vaccination may help, even if it is given to someone who already has long COVID.although it should be noted that in some cases there was a deterioration after such intervention.
Long COVID. How can I help myself?
The good news is that doctors and physical therapists understand the problem better and better. Because without their help, it is often impossible to do. The National Health Fund has launched a special program to help the sick. On the NFZ website you can find the appropriate facility closest to your place of residence.
WHO has in turn made available an online brochure with information on how to help yourself with various types of problems. It is also available in Polish.
Marek Matacz for zdrowie.pap.pl
Ihe mgbu ịhụ nsọ siri ike abụghị mgbe niile “mara mma” ma ọ bụ mmetụta uche nwanyị. Endometriosis nwere ike ịbụ n'azụ mgbaàmà dị otú ahụ. Kedu ihe bụ ọrịa a na kedu ka o si ebi? Gee ntị na pọdkastị gbasara endometriosis nke Patrycja Furs – Endo-girl.