ọdịnaya
Irritable Bowel Syndrome – Medical Treatments
Despite research, medicine does not yet offer anything convincing to treat the akpọnwụ bowel ọrịa. Nowadays it is treated so much on the ọnọdụ uche na na physiological plan, because it is a disorder affecting the interactions between the brain and the digestive system6.
Na-agbanwe gị nri and successfully lowering stress levels can reduce symptoms in mild or moderate cases.
Irritable Bowel Syndrome – Medical Treatments: Understand Everything in 2 Min
When the discomfort is very bothersome, the doctor may prescribe ọgwụ which reduce pain by acting on bowel movements and contractions.
Food
Akwụkwọ ndekọ nri
Before starting a treatment, it is recommended to write down for a few weeks what you eat in order to discover the ihe oriri that systematically trigger discomfort. Then, it is advisable to eliminate problem foods from your menu, or limit their consumption. Advice from a onye na ako nri can be of great help. They will help to find a new, well-adapted and balanced diet.
Some tips to reduce discomfort
- Increase the consumption of soluble eriri, because they are gentle on the intestine: oat cereals, oatmeal, barley and barley cream, for example.
- Belata oriri nke anaghị agbaze eriri, because they stimulate the contractions of the intestine: whole wheat, wheat bran and berries, for example.
- Belata abụba, because they stimulate the contractions of the intestine a lot.
- Limit consumption of foods that can cause bloating and gas. Reactions vary from individual to individual. The foods that are most likely to ferment are milk and dairy products (for lactose intolerant), those that contain sweeteners (for example, sorbitol in sugarless chewing gum) or mannitol ( a sugar-alcohol) and those that contain fructose (such as apples with their skins, figs and dates).
Legumes and crucifers (Brussels sprouts, broccoli, cauliflower, etc.) can also make symptoms worse. It should be noted that it is possible to obtain drugs in pharmacies that absorb excess intestinal gas. Consult our sheet Functional digestive disorders.
jaa. It is recommended for people lactose anabataghị ya eliminate foods containing lactose or take tablets of lactase (eg Lactaid®), the enzyme that breaks down lactose, so as not to deprive the body of an important source of calcium. There are tests that can tell if you are lactose intolerant or not. Ask a nutritionist or your doctor for more information.
- Avoid consuming alcohol, chocolate, coffee, and caffeinated drinks, as they stimulate bowel contractions.
- Replace spices (pepper, chili, cayenne, etc.) with herbs.
- Consume salad and raw vegetables at the end of meals.
- Drink water regularly throughout the day.
- Eat at oge awa, nke ọma chew and don’t skip meals.
For more information, see our Special Diet Irritable Bowel Syndrome fact sheet.
Mbelata nchekasị
Ndi mmadu nchegbu is an aggravating factor should learn to react less to unforeseen and other destabilizing events of daily life, this often helps to regulate the activity of the intestines.
The usoro izu ike have their uses to stop “brooding”, but to really fight stress, we must understand the origin, say the experts. This learning can be done independently or in psychotherapy. Indeed, studies have shown that cognitive-omume akparamaagwa helps reduce symptoms of irritable bowel syndrome1, 29.
Meeting other people with the same problems as you can also help. Group discussions and advice from behavioral medicine specialists can help the person understand their syndrome better and gradually control their symptoms. See the list of Otu na-akwado at the end of this sheet.
The Mayo Clinic also suggests the following approaches to help relax:
– yoga;
– massage therapy;
– meditation.
In addition, makemmega ahụ regularly (30 minutes or more per day) is a good way to relieve stress and fight constipation.
To find out more, see our file on stress.
ọgwụ
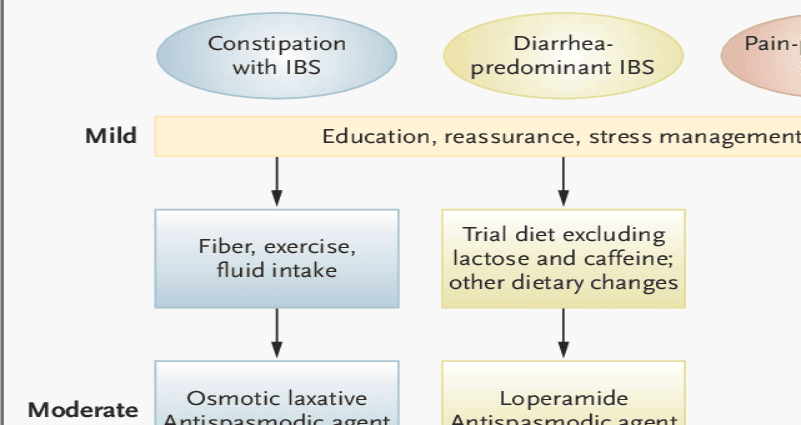
Ụfọdụ ndị nwere ike ịchọ a extra help for their symptoms to subside. The doctor may suggest that they use ọgwụ that contribute to relief.
- Ọ bụrụ na ị nwere a constipation : supplements of ụrọ, also called ballast or bulk laxatives (for example, Metamucil® and Prodiem®), or ihe na -emetụ n'ahụ (which soften the stools) based on docusate sodium (Colace®) or Soflax®) may help. If they have no effect, osmotic laxatives (milk of magnesia, lactulose, Colyte®, Fleet®) can be used. Stimulant laxatives (e.g. Ex-Lax) should only be used in njedebe ikpeazụ, because in the long term, they can interfere with the motility of the intestine.
- Ọ bụrụ na ị nwere a diarrhea: na ihe mgbakwunye eriri often improve stool consistency. They can be tried before using an anti-diarrhea medication. If they do not relieve diarrhea, you can use anti-diarrhea drugs such as loperamide (Imodium®, for example).
- In case of pain: certains antispasmodics (substances that fight spasms) have a direct effect on muscle relaxation, such as pinaverium bromide (Dicetel®, for example) or trimebutine (Modulon®, for example). Others act indirectly, such as dicyclomine and hyoscyamine. When these treatments do not provide relief to the patient, low doses of antidepressants can be used, as they can reduce intestinal sensitivity, especially in people whose main symptom is diarrhea.